
India is deemed the “Diabetes Capital,” with over 100 million people suffering from this deadly disease. The disease is a lifestyle disorder and significantly impacts the quality of life. Thus, the study assesses the lifestyle factors and quality of life (QoL) among people suffering from Type 2 Diabetes (T2D).
A cross-sectional study was conducted among 100 T2DM participants aged 18–65. Data were collected from Diabetic Clinics across Pune City using the Modified Diabetes Quality of Life Questionnaire, having seven domains with 17 questions. Perceived Stress Scale (PSS) and International Physical Activity Questionnaire (IPAQ) were used to assess Stress and Physical Activity. Purposive and snowball sampling techniques were used to collect data. The data was entered and cleaned in Microsoft Excel and analysis was done using SPSS v23. Descriptive and inferential analysis was computed.
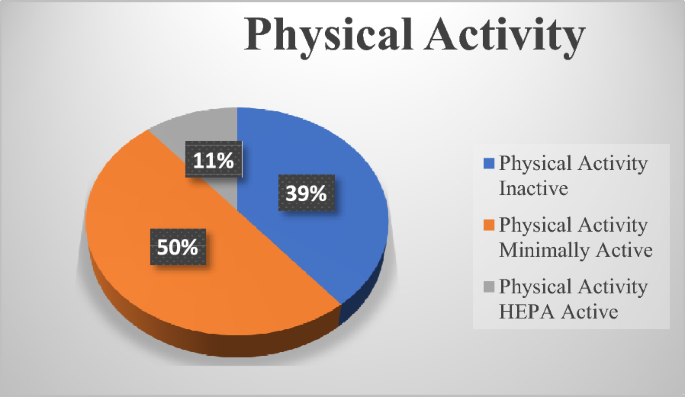
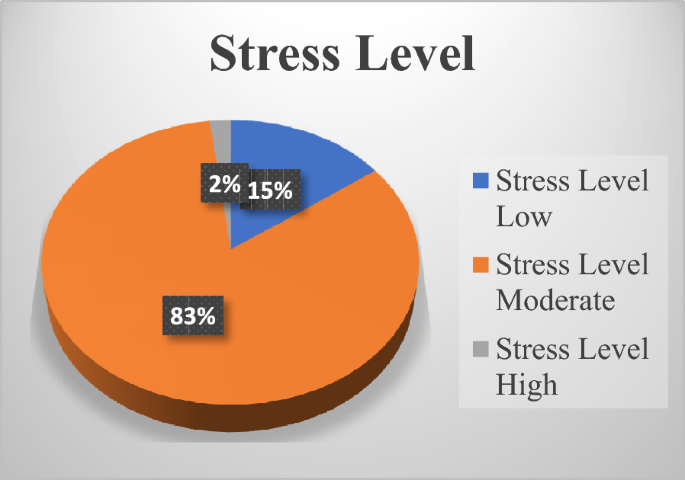
60% of the participants were males with a mean age of 43.30 ± 10.89 years. The mean age of women was 50.17 ± 10.13 years. The mean HbA1c of males and females was 7.98 ± 1.41 and 7.83 ± 1.25, respectively. 83% have moderate stress, while 11% have low stress. Only 11% were found to be physically active. The average QoL score of the participants was 63.4 ± 11.2, non-significantly higher in males than in females (64.9 ± 11.03 vs 61.0 ± 11.22). Domain assessment of QoL showed statistical significance among general health (p = 0.002) and energy fatigue (p = 0.015), with males having better general health than women, and energy levels were better in females than males. However, no significance was seen between the genders in physical function, emotional well-being, and role limitation. A statistical significance for energy fatigue (p = 0.031) was observed when QoL was assessed across the disease duration.
Due to a sedentary lifestyle and increased stress, the glycemic profile of the participants was uncontrolled, which negatively impacted their quality of life. Thus, a holistic approach to managing diabetes will be more beneficial in improving the quality of life.


Avoid common mistakes on your manuscript.
India is deemed the Diabetes Capital of the world, with 101 million people suffering from the disease. The number of affected populations is more in urban than rural areas [1]. Diabetes is a chronic condition that increases the risk of co-morbidities like neuropathy, nephropathy, retinopathy, foot complications, and many more, leading to increased mortality, decreased productivity, and a financial burden [2]. The disease not only affects the physical state but has a significant impact on mental health and is a cause of mental illnesses like anxiety, depression, and stress [3]. Physical and mental health deterioration significantly impacts the patient’s overall quality of life.
QoL describes how well a person leads his or her life. QoL is measured as “physical and social functioning, perceived physical and mental well-being,” as described by WHO [4]. It is a powerful tool to predict a patient’s capacity to manage the disease and maintain long-term health and well-being. QoL depends on several factors, including age, sex, occupation, socioeconomic status, dietary control, exercise regime, the medication used, number of complications, if any, and disease duration [5]. Besides these factors, a sedentary lifestyle and high-calorie and packaged food consumption significantly disturb the patients’ glycemic profile and are also responsible for increasing obesity in these patients [6]. A recent meta-analysis from three cohort studies in the US shows that a 10% increase in ultra-processed food consumption results in a 12% higher risk of developing Type-2 Diabetes (T2D) [7]. Obesity in urban India is 39.6% [1] which is fueled by increasing urbanization, purchase power, and easy availability of packaged and ready-to-eat food [8]. It has also been observed that after the pandemic, stress and anxiety levels in people have increased significantly among women [9]. A cross-sectional study conducted in various parts of India shows that 84% of participants have moderate to severe levels of perceived stress, and 88% have moderate to severe anxiety levels [10]. These factors negatively affect the QoL among diabetic patients.
In the last decade, much attention has been given to QoL as it is considered an essential outcome for diabetes treatment and management. Assessing the QoL of patients at regular intervals at diabetic clinics helps improve health outcomes, identify overlooked problems, and help evaluate the therapeutic effects [11]. The QoL study helps evaluate the overall treatment and care of diabetes and the needs of the patients at different stages of the disease and helps to understand what more has to bring to improve the patient’s help. However, most studies on the Quality of Life showed that Diabetic people have poorer QoL than the healthy population, and the global trend shows that women have poorer QoL than men [12]. Quality of life in diabetic patients is seen to get worse with complications of the disease. A meta-analysis of eighteen studies, 57,109 Type 2 Diabetic patients, shows that complications like neuropathy, retinopathy, presence of hypertension, longer duration of diabetes, depression, and diet with more red meat were associated with poor QoL [13]. Improving glycemic control has been found to reduce morbidity, increase life expectancy, and enhance quality of life for Diabetic patients [14]. Thus, considering all these factors, the study aimed to investigate the QoL of individuals suffering from Diabetes and assess the association across gender, duration of disease, and lifestyle factors affecting the glycemic profile.
This cross-sectional study was conducted from April to May 2023 after approval from the Institutional Ethics Committee. The subjects who meet the inclusion criteria of age 18–65 years, known cases of Type 2 Diabetes, HbA1c ≥ 6.5%, and oral hypoglycemic agents were included. Subjects with Type 1 Diabetes Mellitus (T1DM), Gestational Diabetes Mellitus (GDM), or any recent surgery or hospitalization were excluded from the study. The participants were enrolled by purposive and snowball sampling techniques from Diabetic Clinics across Pune City after obtaining informed consent to participate in the study. The Institutional Ethics Committee of Symbiosis International University (IEC-SIU Pune) approved the study with approval number SIU/IEC/556. The present study has been conducted following the institute’s requirements and Helsinki’s rules.
A pretested questionnaire was used to take the patient’s demographic profile and anthropometric variables, which include height, weight, body mass index (BMI), waist, and hip circumference. Information was also collected about their lifestyle, which included sleep patterns dietary patterns, and consumption of packaged food. The relationship between Diabetes and Sleep disturbances is bidirectional, as poor sleep can elevate blood sugar levels by disturbing circadian rhythm, or factors like hyperglycemia and neuropathy can negatively affect sleep [15]. So, it is important to check this parameter. Self-reported biochemical parameters (tests conducted within the last month) were recorded, including fasting, postprandial blood sugar, and HbA1c levels.
Physical activity levels were assessed using the standard short form of the WHO IPAQ questionnaire [16]. The volume of activity was computed by weighting each type of activity by its energy requirement defined in METS, which are multiples of resting metabolic rates to calculate the score in METS-min. The physical activity was categorized based on METS-min into inactive (less than 500 METS min/week), minimally active (more than 600 METS min/week), and HEPA (Health Enhancing Physical Active) active (minimum 3000 METS min/week) [17]. The Perceived Stress Scale (PSS) developed by Cohen [18] assessed stress levels, which has 10 questions. It is the most widely used physiological instrument for measuring the perception of stress. The question asks about the feelings and thoughts the participants experienced during the last month. Each question was given scores 0–4; the total score was calculated, and based on that, the individual was categorized as having low (0–13 score), moderate (14–26 score), and high stress (27–40 score).
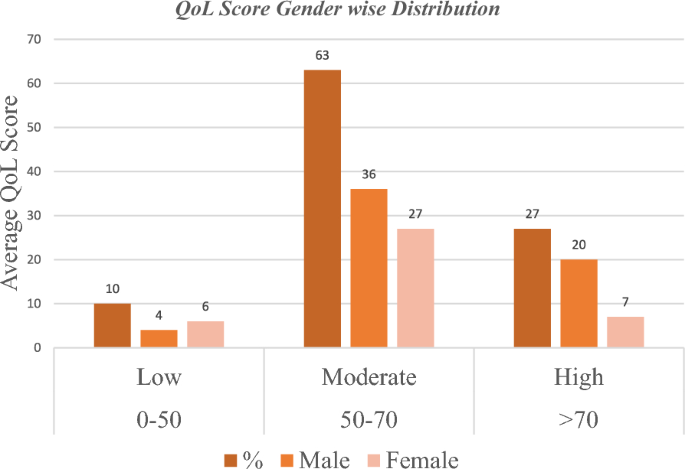
Data on Quality of Life was collected using the Modified Diabetes Quality of Questionnaire (MDQoL), which has already been used and validated in the Indian Diabetic Population [19]. The questionnaire consists of seven domains and 17 questions on General Health, physical functioning, role limitations due to physical health, emotional well-being, role limitations due to emotional problems, social functioning, and energy fatigue. All the responses were scored 0–100, with 0 as the least and 100 as the maximum score. The average total score of all the questions was calculated and based on the QoL score; participants were categorized into low ( < 50), moderate (50–70), and high (>70) [20]. The participants were assessed in all the domains based on gender and the duration of the disease ( < 5 years and >5 years).
The collected data was analyzed using IBM SPSS statistics software, version 23. Descriptive statistics (mean, standard deviation, frequency) were used to express demographic data. An Independent T-test was used for assessing the means of various domains across the groups, and Chi square was used to see the association between the variables. To see the effect of multiple variables of Quality of Life across the gender and duration of Diabetes, Multivariate Analysis of Variance (MANOVA) was performed. Wilk’s lambda, significance, and partial eta square values were used to see the effect. Correlations were performed between different variables using Pearson’s correlation coefficient. A p-value < 0.05 was considered to be significant.
A total of 100 responses were recorded. There were 60% males and 40% females, with a mean age of 46.05 ± 11.07 years. The mean age of males was 43.30 ± 10.89 years, and of females was 50.17 ± 10.13 years. Most participants were above age 40 (60%). Most participants were educated, with 57% being graduates, 29% being post-graduates, and 3% doctorate. Most participants are obese with a mean BMI of 27.53 ± 3.67 kg/m 2 , and are found to have abdominal obesity as the mean waist-to-hip ratio was 0.91 ± 0.05. There was no significant difference in the BMI of males and females. Further analysis revealed that only 8% of participants had normal BMI, 17% were overweight, and 64% were obese (Tables 1 and 2).
The mean QoL score of participants was 63.37 ± 11.21. Males have a slightly better score of 64.93 ± 11.03 than females, 61.02 ± 11.22. About 63% of participants had a moderate score, 27% had a high score, and only 10% were found to have a low score, as shown in Fig. 3. The average QoL score negatively correlates with HbA1c (p = 0.002), as shown in Table 4. The mean QoL score was also calculated across the various domains of QoL and gender, duration of Diabetes as shown in Tables 5 and 6.
Multivariate analysis of variance (MANOVA) is performed to see the significance of quality of life across genders, and the results are summarized in Tables 7 and 8. From multivariate tests (Table 7), it was seen that there was there was no statistical significance among QoL across the genders as F (7,92) = 1.694, p = 0.120 (p > 0.05), Wilk’s Λ = 0.886, partial η 2 = 0.114. Test of between-subject (Table 8) effect shows statistical significance among Energy Fatigue F (1,98) = 6.614, p = 0.015 (p < 0.05), partial η 2 = 0.069, and Gender Health F (1,98) = 10.016, p = 0.002 (p < 0.05), partial η 2 = 0.093 across the gender.
Table 7 Multivariate tests for QoL across the gender Table 8 Tests of between-subjects effects for QoL across the genderWhen comparing the QoL domain with a duration of diabetes (less than 5 years and greater than 5 years of diabetes), through the multivariate test and test of between-subject effects. The results are summarized in Tables 9 and 10. It was found that there was no statistically significant difference in the duration of diabetes and QoL as F (7,92) = 1.076, p > 0.05, Wilk’s Λ = 0.924, partial η 2 = 0.076. When analyzed by the Test of Between-Subject Effect, only a statistical significance is observed with Energy Fatigue Domain and Duration of Diabetes, F (1,98) = 4.76, p = 0.031 (< 0.05), partial η 2 = 0.046.
Table 9 Multivariate tests for QoL across the duration of diabetes Table 10 Tests of between-subjects effects for QoL across the duration of diabetesThe present study is aimed to assess the lifestyle factors and QoL in people with Diabetes in the urban areas of Pune City. A recent study reported that urban areas have a higher prevalence rate of obesity (40%) and Diabetes (16%) as compared to rural areas, wherein the prevalence of obesity was 23.1% and Diabetes was 8.9% [1]. The present study also found the result in a similar context. The mean BMI of the participants in the study falls in the Obese category as per the cut-off for the Asian Population [21]. Abdominal obesity was found to be higher in women than the cut-off value of 0.85, which is in reference to the global trend as women have fat deposited more on the abdomen area.
Dietary habits also help manage blood sugar levels. Many studies favor the consumption of a plant-based diet, which helps effectively manage blood sugar levels. A systematic review of 20 randomized control trials (RCTs) with more than 6 months found that a vegetarian diet showed a more significant body weight reduction, improved glycemic control, and insulin sensitivity [22]. In our study, more than half of the population was found to eat an animal-based diet. Literature suggests that animal protein intensifies insulin resistance, and people who consume animal diets are at more risk for developing Type 2 Diabetes [23]. Eating regularly during the whole day also helps maintain blood sugar levels. A systematic review comparing 14 cohort studies indicates that having breakfast at least 3 times per week has reduced the risk of Type 2 Diabetes Mellitus and Obesity [24]. In our study, 68% of participants had breakfast daily, and more than one-third ate lunch at home. Consumption of ultra-processed food and eating outside food that is high in oil and, sugar, preservatives also increase the risk of Diabetes. A systematic review and meta-analysis involving 18 studies and 1.1 million individuals showed a 72% positive association between ultra-processed food and the risk of Diabetes [25]. We also found that consumption of processed food and eating out at restaurants was high among the participants, either daily or on a weekly basis, intensifying the risk of the disease.
Diabetes is a chronic condition, and its management requires proper care and attention with dietary control and daily physical activity. Doing at least 150 min of moderate to vigorous-intensity activity weekly and not a gap of more than 2 days between the sessions for better glycemic control [26] with only 11% being physically active. Stress also has a prominent role in affecting blood sugar levels. In a healthy individual, any stress releases cortisol, which increases the blood sugar level and is an adaptive response for survival; however, if the stress continues in the long run, it causes insulin resistance and leads to diabetes [27]. The present study also found that 83% of participants have moderate levels of stress. Similar results were found in the study held at a tertiary care hospital in Chennai, India [28]. Sleep is also essential for good health, and people with diabetes frequently struggle with sleep. However, the concept of sleep disturbances has yet to be clearly defined. In our study, 93% of participants reported having irregular sleep, and only 66% reported having adequate sleep of 7–8 h/day. It has also been observed that increased dependency on digital devices resulting in increased screen time has severe adverse effects on physical and mental health. Constant exposure to smartphones, computers, and television affects mental health, increasing stress and anxiety and leading to sleep disorders in children and adults [29]. The study also found comparable results as 93% of participants watched mobile phones, laptops, and television before 1 h of sleep, and 91% had irregular sleep. These all are the critical factors for the dysregulation of blood sugar levels, which in turn affect the QoL of the patients.
The average QoL scores were calculated, and it was found that the mean QoL score of the participants was 63.37 ± 11.21, which was similar to another study by Pham et al. [30]. However, few studies report high QoL Scores [31] and low QoL scores [32]. The variation in results may be attributed to different region participants and the tools used to measure QoL. The results also show that men have slightly better QoL scores than women, consistent with a study conducted across five countries, China, Ghana, India, Russia, and South Africa, with 33,019 participants showing that men have better QoL scores than women [33]. A negative correlation was observed between the QoL score and HbA1c values with p values of 0.002, which indicates that increasing sugar levels affect the quality of life.
The questionnaire has seven domains, including various physical and mental health aspects. A domain-wise analysis between the genders showed that participants scored highest in social functioning and lowest scores in Energy fatigue. Fatigue is a common condition in Diabetes and has a bidirectional relationship; both feed and worsen each other, creating a vicious cycle known as Diabetes Fatigue Syndrome [34]. Our results are consistent with the study by Singh et al. [35] which states that Low energy fatigue scores negatively impact QoL. Thus, it becomes essential for healthcare providers to address fatigue issues during the treatment and management of Diabetes. A statistical significance between the genders is observed, with men complaining that they get fatigued more quickly than women in our study. The reason could be multifactorial as they complain of poor nutritional status, busy work life, sleep irregularity, or mental stress. However, when multivariate analysis was performed, it was seen that despite statistical significance, the partial eta square value was low, which indicates that there was not much effect of energy fatigue on men compared with women. Statistical significance with a p-value of 0.002 is also observed in the Gender Health Domain, with men scoring (59.58 ± 12.44) better than women (49.37 ± 19.82). General Health is a multi-dimensional domain that considers several factors affecting the QoL of the patient. Similarly, the partial eta square value, as seen by the test of between-subject effect, was also low in this case, indicating not much effect among the genders. Many recent studies have shown that the Diabetic population has poor QoL compared to healthy individuals. In most cases, men were observed to have better overall health than women [33, 36]. In the rest of the domains, like role limitation due to physical functioning, emotional well-being, and role limitations due to emotional functioning, there was no statistically significant difference between both genders, indicating that both genders are equally affected.
When comparing the effect of diabetes on the disease duration, a statistical significance (p = 0.031, partial η 2 = 0.046) was found only in the Energy fatigue Domain. The mean score was found to be more (48.66 ± 25.01) with a duration of diabetes of more than 5 years, indicating people who have Diabetes for less than 5 years get fatigued more rapidly than those with Diabetes duration of more than 5 years. However, when multivariate analysis was performed across the duration of diabetes, it was seen that the partial eta square value was less, indicating the effect was not very prominent. Our study results are consistent with the review [37], which states that as the disease progresses, it starts affecting the physiologically (chronic hypo or hyperglycemia) and psychologically (emotional distress and depression related), and thus, Diabetic people complain of fatigue.
In conclusion, our study reveals a commendable level of awareness about dietary management as most participants prefer to eat home-cooked meals, limiting consumption of packaged food to once a week. This indicates a conscientious effort to manage their diet, crucial for blood sugar control. Despite the awareness, most participants were found to be minimally active or inactive, emphasizing the need for improvement in this area as physical activity is a critical component of diabetes management and overall health. A substantial proportion (83%) of participants experience moderate stress. This is concerning, as stress negatively impacts blood sugar levels. Stress management intervention may be beneficial for this population. The quality of life scores among participants was moderate, indicating that while they manage their conditions to some extent, there is room for improvement in their overall well-being. A negative correlation between quality of life scores and HbA1c was observed, meaning that higher blood sugar levels are associated with lower quality of life. This underscores the importance of effective blood sugar management in enhancing the quality of life for people with T2DM. Interestingly, there were no significant differences in the quality of life when compared across the gender and duration of diabetes. This suggests that the impact of diabetes on quality of life is consistent regardless of these factors, indicating that other variables, such as lifestyle and stress, may play a critical role. Based on the results obtained from our study, there is a need to educate people on lifestyle changes that will help them control their glycemic profiles and reduce related complications. Hence, a holistic approach will be vital, which includes team collaboration consisting of a physician, nutritionist, and physiatrist/psychologist to improve the overall quality of life among people suffering from Diabetes.
Data is available with the corresponding author and can be available on request or demand.
The author likes to acknowledge the participants who took their time and gave detailed dietary histories. Also, thank Diabetic Clinics for allowing us to collect the data.
The study received no specific grant from any funding agency.